Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal published online by MDPI (from Volume 28 Issue 1-2021). Established in 1994, the journal represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease. The Canadian Association of Medical Oncologists (CAMO), the Canadian Association of Psychosocial Oncology (CAPO), the Canadian Association of General Practitioners in Oncology (CAGPO), the Cell Therapy Transplant Canada (CTTC), the Canadian Leukemia Study Group (CLSG) and others are affiliated with the journal and their members receive a discount on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 19.8 days after submission; acceptance to publication is undertaken in 2.4 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.8 (2023);
5-Year Impact Factor:
2.9 (2023)
Latest Articles
The Role of [18F]FDG PET/CT Prior to and During Neoadjuvant Chemotherapy for Soft Tissue Sarcomas
Curr. Oncol. 2025, 32(5), 257; https://doi.org/10.3390/curroncol32050257 (registering DOI) - 28 Apr 2025
Abstract
This retrospective, single-center study investigates the association between PET parameters and pathological response or disease recurrence in patients with soft tissue sarcoma (STS) treated with neoadjuvant chemotherapy (NACT). The maximum standardized uptake value (SUVmaxBL), metabolic tumor volume (MTVBL), and
[...] Read more.
This retrospective, single-center study investigates the association between PET parameters and pathological response or disease recurrence in patients with soft tissue sarcoma (STS) treated with neoadjuvant chemotherapy (NACT). The maximum standardized uptake value (SUVmaxBL), metabolic tumor volume (MTVBL), and total lesion glycolysis (TLGBL) were measured at baseline [18F]FDG PET/CT and the change in percentage (ΔSUVmax, ΔMTV, ΔTLG) from baseline to early evaluation [18F]FDG PET/CT was calculated. The optimal cutoff values of the different PET parameters for pathological response, defined as <10% residual viable tumor (RVT) or >15% fibrosis/hyalinization, and recurrence-free survival were obtained for analysis. Forty-two patients who underwent baseline [18F]FDG PET/CT and NACT followed by surgery were included between January 2015 and January 2023. The primary diagnoses were angiosarcoma (n = 15), leiomyosarcoma (n = 15), sarcoma not otherwise specified (n = 9) and synovial sarcoma (n = 3). Twenty-eight (66.6%) patients underwent an early evaluation PET/CT. MTVBL, TLGBL, and ΔSUVmax (p = 0.024; p = 0.042, p = 0.009, respectively) values above the cutoff were associated with a pathological response based on RVT. ΔSUVmax, ΔMTV, and ΔTLG (p = 0.002; p = 0.019; p = 0.039, respectively) values above the cutoff were positively related to >15% fibrosis/hyalinization. MTVBL, TLGBL, and ΔMTV (p = 0.014; p = 0.022; p = 0.034, respectively) values above the cutoff were prognostic for the recurrence of disease. [18F]FDG PET/CT has a promising role in STS patients treated with NACT.
Full article
(This article belongs to the Special Issue Sarcoma Surgeries: Oncological Outcomes and Prognostic Factors)
►
Show Figures
Open AccessSystematic Review
Minimally Invasive Surgical Techniques for Renal Cell Carcinoma with Intravenous Tumor Thrombus: A Systematic Review of Laparoscopic and Robotic-Assisted Approaches
by
Yiting Wu, Shuyang Feng and Ping Fu
Curr. Oncol. 2025, 32(5), 256; https://doi.org/10.3390/curroncol32050256 - 28 Apr 2025
Abstract
Introduction: Locally advanced renal cell carcinoma (RCC) with intravenous tumor thrombus (IVTT) represents 4–10% of renal tumors. This review assesses the safety and outcomes of minimally invasive techniques, specifically laparoscopic (LAP) and robotic-assisted (RA) methods, for treating RCC with IVTT. Methods: A literature
[...] Read more.
Introduction: Locally advanced renal cell carcinoma (RCC) with intravenous tumor thrombus (IVTT) represents 4–10% of renal tumors. This review assesses the safety and outcomes of minimally invasive techniques, specifically laparoscopic (LAP) and robotic-assisted (RA) methods, for treating RCC with IVTT. Methods: A literature search across several databases identified 54 studies (42 case series, 12 cohort studies) for analysis. Perioperative outcomes, including operative time, blood loss, transfusion rates, length of stay, and complications, were compared based on IVTT levels. Results: LAP and RA techniques were feasible for low-level IVTT, showing similar perioperative results. RA outperformed LAP in high-level IVTT with shorter operative times and lower blood loss and transfusion rates, despite managing more complex cases. RA maintained stable cancer-specific mortality (CSM) and metastasis rates, whereas LAP exhibited higher rates in high-level cases. Both techniques had low local recurrence rates. Conclusion: RA may be a superior option for RCC with IVTT, especially in high-level cases, but the data come mainly from specialized centers, signaling a need for multicenter validation and standardized criteria. Long-term outcomes require further study to assess RA’s non-inferiority to LAP.
Full article
(This article belongs to the Section Genitourinary Oncology)
Open AccessArticle
Molecular and Pathological Heterogeneity of Synchronous Small and Large Duct Intrahepatic Cholangiocarcinoma—A Case Series
by
Savelina Popovska, Vladislav Nankov, Boriana Ilcheva and George Dimitrov
Curr. Oncol. 2025, 32(5), 255; https://doi.org/10.3390/curroncol32050255 - 27 Apr 2025
Abstract
Background: Synchronous small- and large-duct intrahepatic cholangiocarcinoma (iCCA) represents a rare and heterogeneous entity, posing challenges for diagnosis, prognosis, and treatment selection. The pathological and molecular diversity between these subtypes influences tumor behavior and therapeutic response, necessitating a personalized approach. This study investigates
[...] Read more.
Background: Synchronous small- and large-duct intrahepatic cholangiocarcinoma (iCCA) represents a rare and heterogeneous entity, posing challenges for diagnosis, prognosis, and treatment selection. The pathological and molecular diversity between these subtypes influences tumor behavior and therapeutic response, necessitating a personalized approach. This study investigates the molecular and pathological heterogeneity of synchronous iCCA and its clinical implications. Methods: This prospective case series included six patients diagnosed with synchronous small- and large-duct iCCA at the Military Medical Academy, Sofia, between January 2023 and January 2025, with a median follow-up of 15 months. Tumor classification was based on histopathological examination, immunohistochemical analysis, and next-generation sequencing (NGS)-based genomic profiling. Radiological and clinical data were analyzed to assess tumor growth patterns, treatment response, and progression-free survival (PFS). Results: Small-duct-predominant iCCA was associated with IDH1/2 mutations and FGFR2 fusions, a mass-forming growth pattern, and longer PFS. In contrast, large-duct-predominant iCCA exhibited KRAS, TP53, and NF1 mutations, an infiltrative periductal growth pattern, and a more aggressive clinical course with shorter PFS. Tumor mutational burden-high (TMB-H) and microsatellite instability-high (MSI-H) were observed in a subset of large-duct iCCA cases, suggesting potential benefit from immune checkpoint inhibitors (ICIs). Conclusions: Synchronous small- and large-duct iCCA demonstrates distinct molecular, histopathological, and clinical features, necessitating individualized treatment strategies. Targeted therapies for IDH1/2- and FGFR2-altered small-duct iCCA have shown efficacy, whereas large-duct iCCA remains more aggressive and treatment-resistant, requiring novel therapeutic approaches. Future research should focus on adaptive treatment strategies that account for tumor heterogeneity and dominant molecular drivers.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures
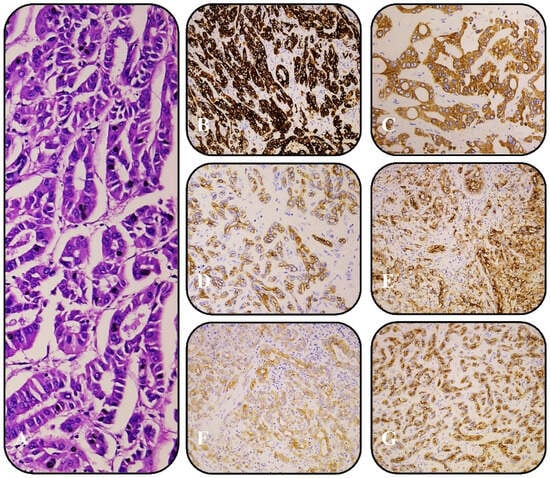
Figure 1
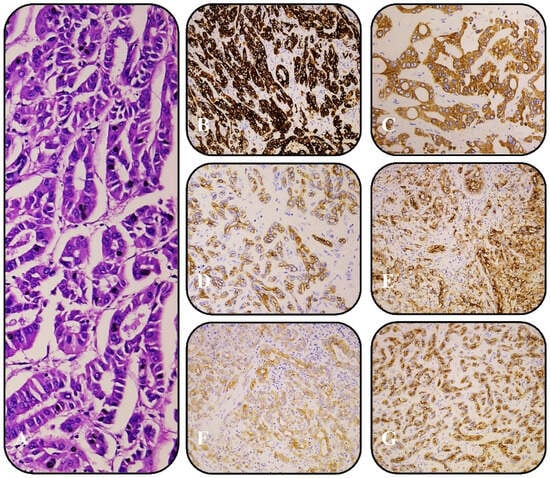
Figure 1
Open AccessArticle
Reassessing the Prognostic Value of Lymph Node Metastasis in Deficient Mismatch Repair Colorectal Cancer
by
Zilan Ye, Dakui Luo, Fan Chen, Jiayu Chen, Zezhi Shan, Junyong Weng, Yu Zhang, Qingguo Li and Xinxiang Li
Curr. Oncol. 2025, 32(5), 254; https://doi.org/10.3390/curroncol32050254 - 27 Apr 2025
Abstract
Background: In non-metastatic deficient mismatch repair (dMMR) colorectal cancer (CRC), traditional prognostic factors, such as pN staging, often fail to distinguish patient outcomes effectively. Methods: This retrospective study included a cohort of 792 dMMR CRC patients who underwent surgical treatment without neoadjuvant chemoradiotherapy
[...] Read more.
Background: In non-metastatic deficient mismatch repair (dMMR) colorectal cancer (CRC), traditional prognostic factors, such as pN staging, often fail to distinguish patient outcomes effectively. Methods: This retrospective study included a cohort of 792 dMMR CRC patients who underwent surgical treatment without neoadjuvant chemoradiotherapy or immunotherapy. Traditional prognostic factors were compared with lymph node-based models (NLN, LNR, LOODS) for their ability to predict overall survival (OS) and disease-free survival (DFS). Results: The study demonstrated that traditional factors, such as histologic type, differentiation, and vascular invasion, had limited predictive value in dMMR CRC. Furthermore, the pN stage failed to effectively distinguish between pN1 and pN2 for both OS (p = 0.219) and DFS (p = 0.095). Conversely, LOODS demonstrated superior performance over traditional pN staging in predicting both OS and DFS (p < 0.001). A prognostic model combining LOODS with age exhibited superior predictive performance compared with the traditional TN staging system. Conclusions: LOODS was identified as a more effective independent prognostic factor compared with traditional pN staging, enabling more precise stratification of pN+ patients in non-metastatic dMMR CRC, highlighting its potential utility in guiding postoperative treatment and optimizing therapeutic strategies.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures
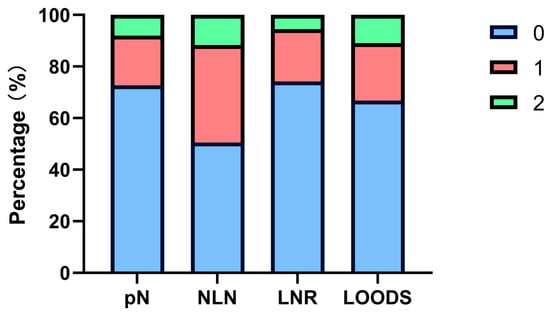
Figure 1
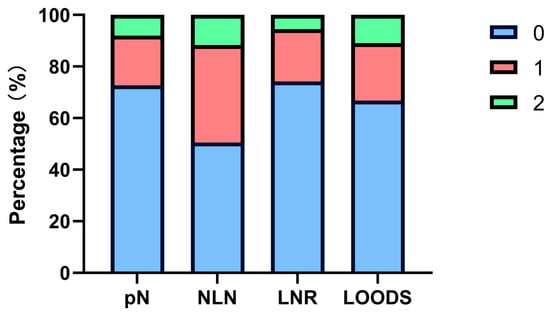
Figure 1
Open AccessArticle
A Multi-Site Refinement Study of Taking Back Control Together, an Intervention to Support Parents Confronted with Childhood Cancer
by
Nikita Guarascio, Ariane Levesque, David Ogez, Valérie Marcil, Daniel Curnier, Véronique Bélanger, Émélie Rondeau, Katherine Péloquin, Caroline Laverdière, Raoul Santiago, Josée Brossard, Stéphanie Vairy, Serge Sultan and The TBCT-Québec Team
Curr. Oncol. 2025, 32(5), 253; https://doi.org/10.3390/curroncol32050253 - 26 Apr 2025
Abstract
A child’s cancer diagnosis profoundly impacts the psychological well-being of parents. To alleviate parental distress, researchers developed Taking Back Control Together (TBCT), a manualized six-session program targeting individual problem-solving skills and dyadic coping. The current study aimed to refine TBCT for future uptake
[...] Read more.
A child’s cancer diagnosis profoundly impacts the psychological well-being of parents. To alleviate parental distress, researchers developed Taking Back Control Together (TBCT), a manualized six-session program targeting individual problem-solving skills and dyadic coping. The current study aimed to refine TBCT for future uptake across different sites. We invited potential interventionists and local stakeholders from three pediatric oncology centers (CHU Sainte-Justine, CHU de Sherbrooke, and CHU de Québec) to join the refinement team. The final working team comprised 26 professionals, including social workers, psychologists, researchers, coordinators, and parent-partners. The study included eight 50- to 90-min discussion sessions designed to stimulate conversation and facilitate the exchange of ideas and perspectives. We used framework analysis to identify and describe patterns within the qualitative data. The data were organized into three categories: (1) intervention description, which addresses changes in personnel, modes of delivery, and tailoring to accommodate different family structures; (2) content modifications, which include language simplification and visual enhancements; and (3) factors influencing TBCT’s future uptake, such as accessibility, participant satisfaction, clinician compensation, and flexibility in program delivery. The direct output of this research is a refined program with an updated manual, tools, and format adapted for use in different sites.
Full article
(This article belongs to the Section Childhood, Adolescent and Young Adult Oncology)
Open AccessArticle
The Application Effect of Endoscopic Thyroidectomy via the Gasless Unilateral Axillary Approach in Thyroid Cancer and Its Impact on Postoperative Stress Response
by
Jinliang Jia, Jihua Han, Rui Pang, Wen Bi, Bo Liu, Ruinan Sheng and Lingyu Kong
Curr. Oncol. 2025, 32(5), 252; https://doi.org/10.3390/curroncol32050252 - 26 Apr 2025
Abstract
Objective: This study aims to evaluate the application effect of endoscopic thyroidectomy via the gasless unilateral axillary (GUA) approach in thyroid cancer and its impact on the postoperative stress response. Methods: Ninety-four thyroid cancer patients were enrolleod and assigned into the open group
[...] Read more.
Objective: This study aims to evaluate the application effect of endoscopic thyroidectomy via the gasless unilateral axillary (GUA) approach in thyroid cancer and its impact on the postoperative stress response. Methods: Ninety-four thyroid cancer patients were enrolleod and assigned into the open group (underwent conventional-open-anterior-cervical-approach thyroidectomy) and the endoscopic group (underwent GUA endoscopic thyroidectomy) (n = 47). Perioperative indicators between the two groups were compared. Thyroid function parameters [total triiodothyronine (TT3), total thyroxine (TT4), free triiodothyronine (FT3), free thyroxine (FT4), and thyroid-stimulating hormone (TSH)] were measured preoperatively and on postoperative day 2. Inflammatory markers [interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α)] and stress-related hormones [norepinephrine (NE) and cortisol (Cor)] were evaluated preoperatively and on postoperative day 1. The aesthetic appearance of the incision was evaluated at 1 and 3 months postoperatively using the Vancouver Scar Scale (VSS). Postoperative complications were also compared between the two groups. Results: The endoscopic group exhibited less intraoperative blood loss, reduced postoperative drainage, a lower pain degree on 1 day postoperatively, a shorter hospitalization time, and a longer surgical time versus the open group (p < 0.05). The serum levels of TT3, TT4, FT3, and FT4 were lower, while the TSH levels were higher in both groups on postoperative day 2 compared to preoperative values. Additionally, the serum levels of IL-6, TNF-α, NE, and Cor increased on day 1 postoperatively, with the endoscopic group showing lower levels of these markers compared to the open group (p < 0.05). The VSS scores at 1 and 3 months after surgery were lower in the endoscopic group compared to the open group, indicating better cosmetic outcomes (p < 0.05). The incidence of postoperative complications was comparable between the endoscopic and open groups (p > 0.05). Conclusions: Endoscopic thyroidectomy by a GUA offers notable advantages over the conventional-open-anterior-cervical-approach thyroidectomy, including reduced intraoperative blood loss, less postoperative drainage, and a lower postoperative stress response. This approach also results in improved cosmetic outcomes, making it a promising alternative for thyroid cancer surgery.
Full article
(This article belongs to the Section Head and Neck Oncology)
Open AccessSystematic Review
Molecular Prognostic Factors in Uterine Serous Carcinomas: A Systematic Review
by
Anna Svarna, Michalis Liontos, Alkistis Papatheodoridi, Aristea-Maria Papanota, Eleni Zografos, Maria Kaparelou, Flora Zagouri and Meletios-Athanasios Dimopoulos
Curr. Oncol. 2025, 32(5), 251; https://doi.org/10.3390/curroncol32050251 - 25 Apr 2025
Abstract
Uterine serous carcinomas are an aggressive minority of endometrial cancers. They are characterized by mutations in TP53 and extensive copy number alterations and are primarily classified in the copy number-high/p53abn molecular prognostic group, highlighting a unique molecular profile that is crucial for understanding
[...] Read more.
Uterine serous carcinomas are an aggressive minority of endometrial cancers. They are characterized by mutations in TP53 and extensive copy number alterations and are primarily classified in the copy number-high/p53abn molecular prognostic group, highlighting a unique molecular profile that is crucial for understanding their behavior and treatment responses. Clinical studies have shown that molecular categorization via biomarkers can facilitate proper treatment selection, and this is now widely used. In this context, the scope of this systematic review is to identify molecular characteristics with prognostic significance for these neoplasms to further inform on their treatment needs. We performed a comprehensive literature search of all articles written in English using the PubMed/Medline and Cochrane databases through February 2025. Our review led to the inclusion of 95 studies, from which we identified a total of 66 distinct molecular characteristics along with new cancer signatures that may impact prognosis. These findings have the potential to inform clinical practice by aiding in the development of tailored treatment strategies for patients with uterine serous carcinoma, ultimately improving outcomes in this challenging malignancy.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Delayed Bronchopleural Fistula Formation Following Salvage Surgery of Stage IV Anaplastic Lymphoma Kinase-Positive Non-Small-Cell Lung Cancer
by
Lauren Barter, Stephanie Snow, Aneil Mujoomdar, Lara Best and Daniel French
Curr. Oncol. 2025, 32(5), 250; https://doi.org/10.3390/curroncol32050250 - 25 Apr 2025
Abstract
This case report highlights the management of a delayed bronchopleural fistula (BPF) following salvage pulmonary resection to achieve local control and no radiographic evidence of disease in a patient treated with serial tyrosine kinase inhibitors (TKIs) for stage IV anaplastic lymphoma kinase (ALK)-positive
[...] Read more.
This case report highlights the management of a delayed bronchopleural fistula (BPF) following salvage pulmonary resection to achieve local control and no radiographic evidence of disease in a patient treated with serial tyrosine kinase inhibitors (TKIs) for stage IV anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer (NSCLC). The initial pulmonary resection was complicated by dense adhesions and an abnormally torturous pulmonary artery. Six weeks after the index surgery, the patient presented with a delayed BPF requiring decortication, repair of airway, and coverage of the bronchial stump with a serratus anterior muscle flap.
Full article
(This article belongs to the Special Issue Clinical Management and Outcomes of Lung Cancer Patients)
►▼
Show Figures
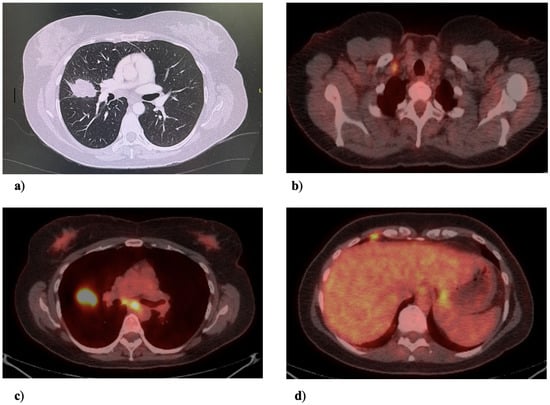
Figure 1
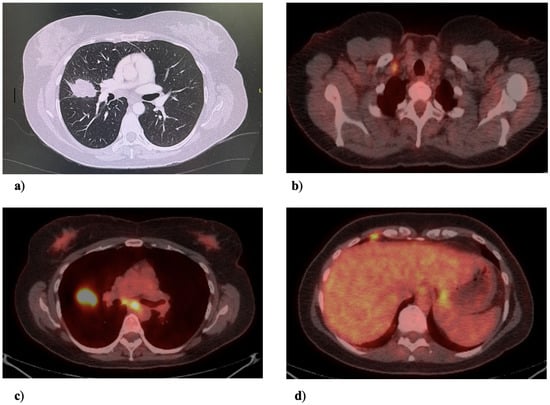
Figure 1
Open AccessCommentary
Current and Future Directions Using Virtual Avenues for Care Delivery Across the Cancer Continuum
by
Charlotte T. Lee, Franco Ng and Elizabeth Borycki
Curr. Oncol. 2025, 32(5), 249; https://doi.org/10.3390/curroncol32050249 - 24 Apr 2025
Abstract
Oncology nurses have long been at the forefront of virtual care, transitioning from telenursing to technology-driven delivery methods that address the evolving needs of cancer patients. Initially developed to overcome barriers to care for rural and underserved populations, virtual care has grown into
[...] Read more.
Oncology nurses have long been at the forefront of virtual care, transitioning from telenursing to technology-driven delivery methods that address the evolving needs of cancer patients. Initially developed to overcome barriers to care for rural and underserved populations, virtual care has grown into a critical component of oncology practice. Oncology nurses play a central role in providing timely, personalized, and holistic care, leveraging tools such as remote monitoring, patient-reported outcomes, and mHealth platforms. However, the rapid adoption of virtual care demands a broader focus to sustain its impact. This commentary explores the need to clearly define the role of oncology nurses in virtual care, emphasizing leadership in digital health, the integration of hybrid care models, and workforce training. By addressing these priorities, virtual care can continue to enhance patient outcomes, strengthen nursing-led interventions, and expand the scope of oncology nursing, positioning it as an essential and enduring facet of cancer care delivery.
Full article
(This article belongs to the Special Issue Feature Reviews in Section "Oncology Nursing")
Open AccessArticle
The Influence of Poverty and Rurality on Colorectal Cancer Survival by Race/Ethnicity: An Analysis of SEER Data with a Census Tract-Level Measure of Persistent Poverty
by
Steven S. Coughlin, Meng-Han Tsai, Jorge Cortes, Malcolm Bevel and Marlo Vernon
Curr. Oncol. 2025, 32(5), 248; https://doi.org/10.3390/curroncol32050248 - 23 Apr 2025
Abstract
Purpose: Because of shared mechanisms such as decreased access to health care, rurality and poverty may act synergistically to decrease colorectal cancer (CRC) survival. Methods: We conducted a retrospective cohort analysis of SEER data (22 registries) with census tract-level measures of poverty/rurality for
[...] Read more.
Purpose: Because of shared mechanisms such as decreased access to health care, rurality and poverty may act synergistically to decrease colorectal cancer (CRC) survival. Methods: We conducted a retrospective cohort analysis of SEER data (22 registries) with census tract-level measures of poverty/rurality for the period 2006–2015. Multivariable Cox proportional hazard regressions were applied to examine the independent and intersectional associations of persistent poverty and rurality on 5-year cause-specific CRC survival across five racial/ethnic groups. Results: Among 532,868 CRC patients, non-Hispanic Blacks (NHB) demonstrated lower 5-year survival probability (64.2% vs. 68.3% in non-Hispanic Whites [NHW], 66.5% in American Indian/Alaska Natives [AI/AN], 72.1% in Asian/Pacific Islanders, and 68.7% in Hispanic groups) (p-value < 0.001). In adjusted analysis, CRC patients living in rural areas with poverty were at a 1.2–1.6-fold increased risk of CRC death than those who did not live in these areas in five racial/ethnic groups. In particular, AI/AN patients living in rural areas with poverty were 66% more likely to die from CRC (95% CI, 1.32, 2.08). Conclusions: CRC patients who live in rural or poverty areas in SEER areas in the U.S. have a poorer survival compared with those who do not live in such areas regardless of race/ethnicity. Significantly greater risk of CRC death was observed in AI/ANs. Impact: Patient navigators, community education or screening, and other health care system interventions may be helpful to address these disparities by socioeconomic status, race, and geographic residence. Multi-level interventions aimed at institutional racism and medical mistrust may also be helpful.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures
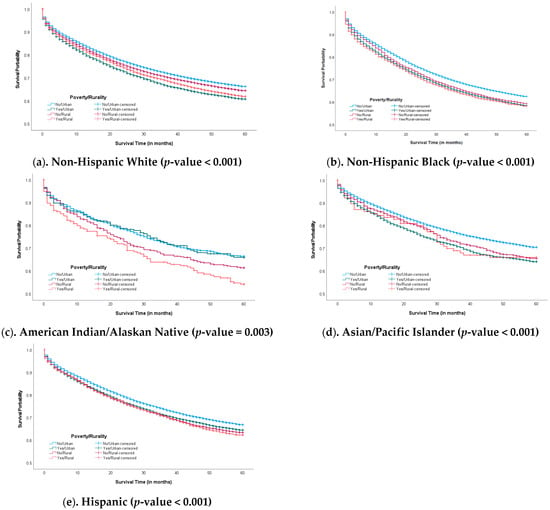
Figure 1
Open AccessArticle
COVID-19 Pandemic’s Effects on Breast Cancer Screening, Staging at Diagnosis at Presentation, Oncologic Management, and Immediate Reconstruction: A Canadian Perspective
by
Adolfo Alejandro Lopez Rios, Alissa Dozois, Alexander T. Johnson, Toros Canturk and Jing Zhang
Curr. Oncol. 2025, 32(5), 247; https://doi.org/10.3390/curroncol32050247 - 23 Apr 2025
Abstract
Background: Did the COVID-19 pandemic lead to delays in breast cancer management, impacting treatment recommendations? The goal of this study was to assess the pandemic’s effect on breast cancer treatment and management practices. Methods: This study aimed to assess the pandemic’s effect on
[...] Read more.
Background: Did the COVID-19 pandemic lead to delays in breast cancer management, impacting treatment recommendations? The goal of this study was to assess the pandemic’s effect on breast cancer treatment and management practices. Methods: This study aimed to assess the pandemic’s effect on breast cancer treatment from March 2018 to February 2020 (pre-pandemic) and March 2020 to February 2022 (during the pandemic) in Canada. A retrospective cohort study at The Ottawa Hospital, Ontario, Canada, compared breast cancer patients diagnosed in the two years before and after the pandemic’s onset. The study examined patient demographics, cancer stages, treatment timelines, and procedures, including neoadjuvant chemotherapy, endocrine therapy, and surgical treatment. Descriptive statistics and frequencies identified changes. The study is limited to a single institution, which may restrict generalizability. Inclusion criteria focused on female patients over 18 years with newly diagnosed breast cancer, excluding recurrent cases. Stage IV patients were included, but further details on their management are needed. Results: Breast cancer diagnoses decreased from 2577 before the pandemic to 2290 after its onset. Surgeries decreased from 1226 to 1013 (p < 0.020), while neoadjuvant endocrine therapy increased from 148 to 169, and adjuvant radiotherapy rose from 586 to 722 (p < 0.001). The study revealed a decrease in breast cancer diagnoses and surgeries during the pandemic, with a rise in non-surgical treatments. Conclusions: These changes indicate significant shifts in breast cancer management due to the pandemic. The decrease in surgical treatments and increase in non-surgical options such as endocrine therapy and radiotherapy suggest adaptations in clinical practices to cope with the challenges posed by the pandemic. Understanding these shifts is crucial for developing strategies to mitigate the impact of future disruptions on breast cancer care and ensuring optimal patient outcomes.
Full article
(This article belongs to the Section Breast Cancer)
Open AccessArticle
Use of Radiofrequency in Robot-Assisted Partial Nephrectomy for Small Tumors: A Novel Technique
by
Matías Larrañaga, Helga Ibañez, Jessica Pfeifer, Cristobal Román, Rubén Olivares, José Antonio Salvadó, José Miguel Cabello, Sergio Moreno, Renato Cabello, Carmen Franco and Alfredo Velasco
Curr. Oncol. 2025, 32(5), 246; https://doi.org/10.3390/curroncol32050246 - 23 Apr 2025
Abstract
Introduction and Objectives: Radiofrequency is standardized for ablating small renal tumors, but evidence regarding its effects remains limited. Partial nephrectomy, the gold standard, often leads to hemorrhagic complications and irreversible renal damage due to hilum clamping. To mitigate these risks, we propose a
[...] Read more.
Introduction and Objectives: Radiofrequency is standardized for ablating small renal tumors, but evidence regarding its effects remains limited. Partial nephrectomy, the gold standard, often leads to hemorrhagic complications and irreversible renal damage due to hilum clamping. To mitigate these risks, we propose a novel technique that replaces clamping with radiofrequency ablation of the tumor for hemostasis in robot-assisted partial nephrectomy. Methods: We report on 357 consecutive patients with T1a renal tumors treated with robot-assisted surgery between 2010 and July 2024. Radiofrequency was used peri-tumorally for hemostasis, followed by complete lesion enucleation. Follow-up included ultrasound and creatinine at 1 month, CT scans at months 3 and 9, and then annually for 5 years. Results: The median age was 60.2 years, with 251 men (70.3%). The median tumor size was 22 mm, and the median blood loss was 15 mL. Hemorrhagic complications occurred in eight patients (2.2%), with one requiring a blood transfusion (0.28%). A total of 30 patients experienced transient stage 1 acute kidney disease (8.4%), with no significant change in median 74.92 mL/min/1.77 m2 vs. 78.77 mL/min/1.77 m2 vs. (p-value 0.15). The median follow-up was 48.2 months, with no tumor recurrence at the treated site. Renal cell carcinoma was found in 83.7% of tumors. Conclusions: To our knowledge, this series represent the largest global undertaking of renal tumor treatment using peripheral radiofrequency ablation without clamping, demonstrating optimal surgical and oncological outcomes, lower morbidity, and fewer complications compared to those noted in the revised literature regarding traditional clamping techniques.
Full article
(This article belongs to the Section Surgical Oncology)
►▼
Show Figures
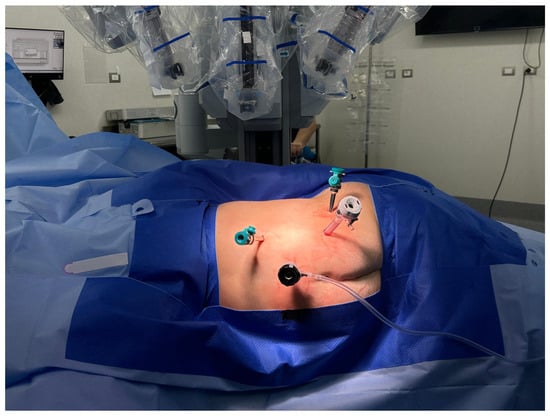
Figure 1
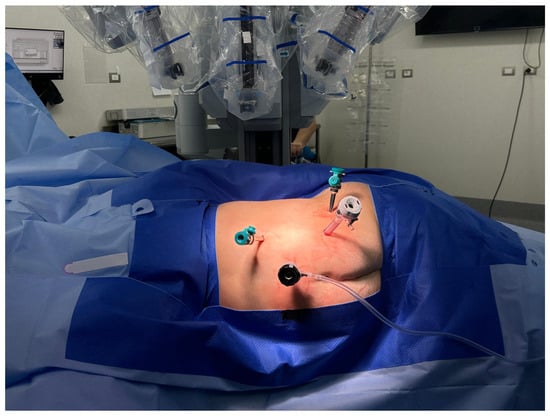
Figure 1
Open AccessArticle
Prognosis of Cancer Patients with Severe Hyponatremia in the Emergency Department: A Retrospective Study from the National Cancer Center of China
by
Qinglong Jiang, Xi Zhang, Chao Wang, Rong Qin, Rui Sun, Shengling Qin, Cong Zhao, Zhiyong Li, Wenjie Zhu and Minghua Cong
Curr. Oncol. 2025, 32(5), 245; https://doi.org/10.3390/curroncol32050245 - 23 Apr 2025
Abstract
Aim: The aim of this study was to analyze the clinical characteristics and prognostic factors of profound hyponatremia in solid cancer patients admitted to the oncologic emergency department. Methods: We gathered data retrospectively from cancer patients who visited the emergency department of the
[...] Read more.
Aim: The aim of this study was to analyze the clinical characteristics and prognostic factors of profound hyponatremia in solid cancer patients admitted to the oncologic emergency department. Methods: We gathered data retrospectively from cancer patients who visited the emergency department of the National Cancer Center of China between October 2019 and February 2023 with a serum sodium (Na) level of less than 125 mmol/L. The demographic and clinical characteristics, medical history, admission symptoms, laboratory parameters, and outcomes of the patients were recorded. Results: This study comprised 307 patients with severe hyponatremia in total. With 39.4% of all tumors being lung cancer (n = 121), nausea and vomiting were the most common admission symptoms for patients with severe hyponatremia. The 30-day mortality rate of profound hyponatremia cancer patients in the emergency department was 13.4%. The albumin level (p < 0.001), the hemoglobin level (p = 0.033), the TNM stage (p = 0.004), the Eastern Cooperative Oncology Group Performance Status (ECOG-PS) score (p < 0.001), hypocalcemia (p = 0.006), renal insufficiency (p = 0.035), and the efficacy of sodium supplementation (p = 0.006) were significantly associated with 30-day mortality. Binary logistic regression analysis showed that a lower albumin level (OR 0.924, 95% CI 0.861–0.991, p = 0.028) and higher ECOG score (OR 8.443, 95% CI 3.568–19.976, p < 0.001) were independent risk factors for 30-day mortality. The overall survival of emergency cancer patients with severe hyponatremia was also examined. The results of the COX regression analysis demonstrated that the efficacy of sodium supplementation (OR = 2.643, 95% CI 1.593–4.386, p < 0.001), a low albumin level (OR = 0.654, 95% CI 0.463–0.923, p = 0.016), the TNM stage (OR = 4.606, 95% CI 2.846–7.455), and a higher ECOG score (OR = 1.738, 95% CI 1.292–2.338, p < 0.001) were independent risk factors for overall survival. Conclusions: The clinical manifestations of severe hyponatremia in emergency cancer patients are varied. Hypoalbuminemia and a higher ECOG score are independent risk factors for 30-day mortality and overall survival. Severe hyponatremia patients with a high ECOG score and/or a low albumin level should be monitored and followed more closely.
Full article
(This article belongs to the Section Palliative and Supportive Care)
►▼
Show Figures

Figure 1

Figure 1
Open AccessReview
Technical Innovations and Complex Cases in Robotic Surgery for Lung Cancer: A Narrative Review
by
Giacomo Cusumano, Giuseppe Calabrese, Filippo Tommaso Gallina, Francesco Facciolo, Pierluigi Novellis, Giulia Veronesi, Stefano Viscardi, Filippo Lococo, Elisa Meacci, Alberto Terminella, Gaetano Romano, Cristina Zirafa, Franca Melfi, Stefano Margaritora and Marco Chiappetta
Curr. Oncol. 2025, 32(5), 244; https://doi.org/10.3390/curroncol32050244 - 22 Apr 2025
Abstract
For over two decades, robotic-assisted thoracic surgery (RATS) has revolutionized thoracic oncology. With enhanced visualization, dexterity, and precision, RATS has reduced blood loss, shortened hospital stays, and sped up recovery compared to traditional surgery or video-assisted thoracoscopic surgery (VATS). The use of 3D
[...] Read more.
For over two decades, robotic-assisted thoracic surgery (RATS) has revolutionized thoracic oncology. With enhanced visualization, dexterity, and precision, RATS has reduced blood loss, shortened hospital stays, and sped up recovery compared to traditional surgery or video-assisted thoracoscopic surgery (VATS). The use of 3D high-definition imaging and articulated instruments allows for complex resections and advanced lymph node assessment. RATS delivers oncological outcomes similar to open surgery and VATS, with high rates of complete (R0) resections and acceptable complication rates. Its minimally invasive nature promotes quicker recovery. Advances in imaging software and augmented reality further enhance surgical accuracy and reduce intraoperative risks. However, RATS has some limitations, including high costs and a lack of tactile feedback, and certain complex procedures, such as extended resections and intrapericardial interventions, remain challenging. With growing experience and technological advances, RATS shows promise in reducing morbidity, improving quality of life, and expanding access to advanced oncologic care. This article reviews the evolution, benefits, and limitations of RATS in NSCLC treatment, highlighting its emerging role in managing complex cases.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures
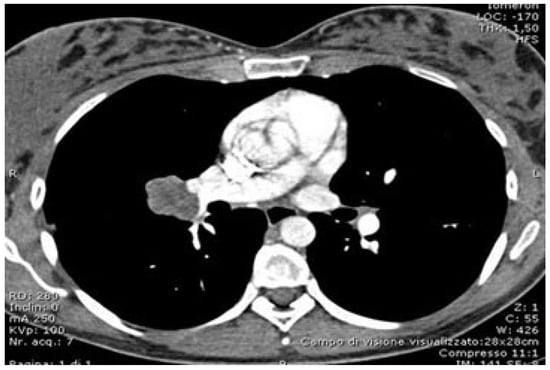
Figure 1
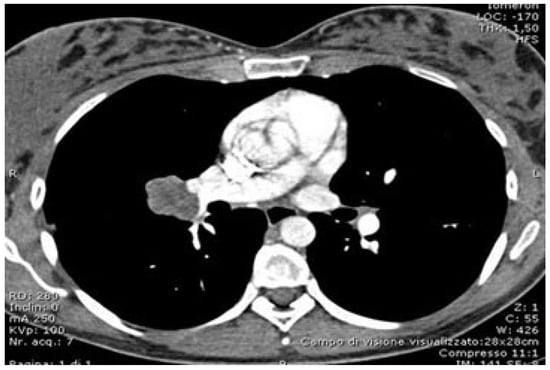
Figure 1
Open AccessArticle
Predictors of Colon Cancer Screening Among the Saudi Population at Primary Healthcare Settings in Riyadh
by
Amani Alharthy, Mamdouh M. Shubair, Badr F. Al-Khateeb, Lubna Alnaim, Emad Aljohani, Nada Kareem Alenazi, Maha Alamodi Alghamdi, Khadijah Angawi, Rawabi M. Alsayer, Naif M. Alhawiti and Ashraf El-Metwally
Curr. Oncol. 2025, 32(5), 243; https://doi.org/10.3390/curroncol32050243 - 22 Apr 2025
Abstract
(1) Background: This study aims to identify the sociodemographic, behavioural, and systemic predictors of colorectal cancer (CRC) screening among primary healthcare attendees in Riyadh, Saudi Arabia, to inform targeted interventions and policy strategies. (2) Methods: This cross-sectional study was conducted between March and
[...] Read more.
(1) Background: This study aims to identify the sociodemographic, behavioural, and systemic predictors of colorectal cancer (CRC) screening among primary healthcare attendees in Riyadh, Saudi Arabia, to inform targeted interventions and policy strategies. (2) Methods: This cross-sectional study was conducted between March and July 2023 across 48 randomly selected primary healthcare centers in Riyadh, Saudi Arabia. The target population for this study was adults aged 18 and above attending primary healthcare centers in Riyadh. Multi-stage random sampling was used to recruit participants. Multivariate logistic regression was performed to identify independent predictors of CRC screening. (3) Results: CRC screening uptake was found to be only 4.2%. Age was a significant predictor, with individuals aged 50–75 years (adjusted odds ratio [AOR]: 1.90, 95% confidence interval [CI]: 1.50–2.42) and those aged 75 years or older (AOR: 1.37, 95% CI: 1.01–1.87) being more likely to undergo screening compared to younger individuals. Insurance coverage strongly influenced screening behaviour (AOR: 1.64, 95% CI: 1.37–1.96). Smokers were nearly four times more likely to participate in screening than non-smokers (AOR: 3.87, 95% CI: 3.21–4.69), and physical activity was positively associated with screening (AOR: 1.43, 95% CI: 1.11–1.82). (4) Conclusions: CRC screening uptake in Riyadh is critically low, highlighting the need for targeted public health interventions. Key predictors such as age, insurance coverage, smoking, and physical activity underscore the importance of addressing sociodemographic disparities and promoting health awareness. The findings emphasize the need for culturally tailored educational campaigns, improved healthcare access, and enhanced screening programs to increase uptake.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
Open AccessReview
Glioblastoma in NF1: A Unique Entity—A Literature Review Focusing on Surgical Implication and Our Experience
by
Elisa Garbin, Lorenzo Nicolè, Salima Magrini, Yuri Ceccaroni, Luca Denaro, Luca Basaldella and Marta Rossetto
Curr. Oncol. 2025, 32(4), 242; https://doi.org/10.3390/curroncol32040242 - 21 Apr 2025
Abstract
Glioblastoma in patients affected by NF1 germline mutation (NF1-associated GBM) represents a unique heterogeneous clinical and pathological entity. We have reviewed the few cases reported in the literature and they seem to have a better response to standard therapy and overall survival than
[...] Read more.
Glioblastoma in patients affected by NF1 germline mutation (NF1-associated GBM) represents a unique heterogeneous clinical and pathological entity. We have reviewed the few cases reported in the literature and they seem to have a better response to standard therapy and overall survival than GBM in the non-NF1 population. We present two cases of long-survival NF1 patients with GBM. Case 1 was a 38-year-old woman with cerebellar GBM who underwent surgical asportation and the Stupp protocol many times with an overall survival of 117 months. Case 2 was a 47-year-old woman with GBM in the eloquent area of the right frontal lobe; she underwent surgical asportation and the Stupp protocol with an overall survival of 25 months. The data analysis demonstrates that NF1-associated GBM patients could be considered long-term survivors.
Full article
(This article belongs to the Special Issue Treatment for Glioma: Retrospect and Prospect)
►▼
Show Figures
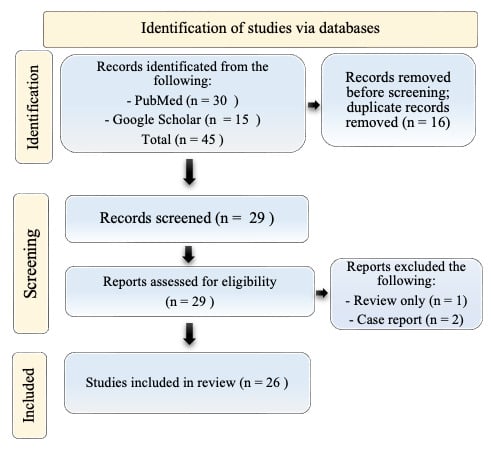
Figure 1
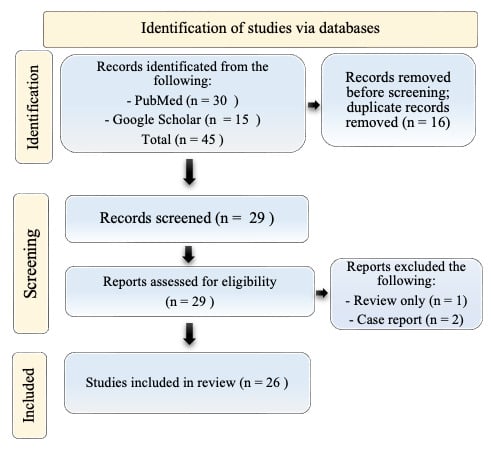
Figure 1
Open AccessConference Report
40th Annual CAPO Conference—Responding to the Human Experience of Cancer and Caring for the Soul: Building on 40 Years of Global Leadership in Psychosocial Oncology
by
Peter Traversa and Doris Howell
Curr. Oncol. 2025, 32(4), 241; https://doi.org/10.3390/curroncol32040241 - 20 Apr 2025
Abstract
On behalf of the Canadian Association of Psychosocial Oncology, we are pleased to present the Abstracts from the 2025 Annual Conference, titled “Responding to the Human Experience of Cancer and Caring for the Soul: Building on 40 years of global leadership in psychosocial
[...] Read more.
On behalf of the Canadian Association of Psychosocial Oncology, we are pleased to present the Abstracts from the 2025 Annual Conference, titled “Responding to the Human Experience of Cancer and Caring for the Soul: Building on 40 years of global leadership in psychosocial oncology”. The 40th Annual CAPO Conference was held in Toronto from 23 April 2025 to 25 April 2025. In an era marked by the rapid advancement of biologically focused precision medicine, it is imperative to redirect our attention towards the human experience of illness and the soul of medicine. Biomedicine has conceptualized illness in ways that have proved profoundly productive from a curative and biological point of view. But it cannot—and it does not pretend to—illuminate the experience of living with it. (Hurwitz 2009). This conference aims to delve into the intricate interplay between cutting-edge biomedical technologies inclusive of artificial intelligence and big data and the deeply personal narratives of individuals navigating illness. By shifting the focus from mere disease pathology to encompassing the holistic human experience, we aspire to foster a more compassionate and patient-centered approach to healthcare with psychosocial support at the core of humanistic care that can improve survival and well-being in all aspects of a whole-person approach to illness. Through interdisciplinary dialogue and introspection, we endeavor to illuminate the profound connection between mind, body, and spirit in the practice of medicine, reaffirming the timeless significance of empathy, understanding, and human connection in healing and psychosocial aspects of care as fundamental to living well with cancer. This conference brought together key stakeholders including multidisciplinary professionals from nursing, psychology, psychiatry, social work, spiritual care, nutrition, medicine, rehabilitation medicine, occupational health and radiation therapy for both adult and pediatric populations. Participants included clinicians, researchers, educators in cancer care, community-based organizations and patient representatives. Patients, caregivers and family members presented abstracts that speak to their role in managing cancer experiences and care. Over two hundred (200) abstracts were submitted for presentation as symposia, 20-minute oral presentations, 10-minute oral presentations, 90-minute workshops and poster presentations. We congratulate all the presenters on their research work and contribution.
Full article
(This article belongs to the Section Psychosocial Oncology)
Open AccessArticle
Cost-Effectiveness Analysis of Contemporary Advanced Prostate Cancer Treatment Sequences
by
Valentyn Litvin, Armen G. Aprikian and Alice Dragomir
Curr. Oncol. 2025, 32(4), 240; https://doi.org/10.3390/curroncol32040240 - 20 Apr 2025
Abstract
There has been a proliferation of novel treatments for the management of advanced prostate cancer (PCa), including androgen receptor pathway inhibitors (ARPI). Although there are health economic analyses of novel PCa treatments, such as ARPIs for specific health states, there is a lack
[...] Read more.
There has been a proliferation of novel treatments for the management of advanced prostate cancer (PCa), including androgen receptor pathway inhibitors (ARPI). Although there are health economic analyses of novel PCa treatments, such as ARPIs for specific health states, there is a lack of sequential analyses. Our paper aims to fill this gap. We developed a Monte Carlo Markov model to simulate the management of advanced PCa to end-of-life. We modeled patients who begin in metastatic and nonmetastatic castration-sensitive PCa (mCSPC and nmCSPC), with risk stratification for mCSPC, progressing to metastatic castration-resistant PCa (mCRPC). Using current guidelines and recent literature, we simulated admissible treatment sequences over these states along a 15-year horizon. We report the best treatment sequences in terms of efficacy and cost-effectiveness. We find that the most cost-effective use of ARPIs is early in advanced PCa for a cost-effectiveness threshold (CET) of CAD 100K per QALY. For a CET of CAD 50K per QALY, early ARPI use is most cost-effective in mCSPC-starting patients but not nmCSPC-starting. We conclude that the most cost-effective way to use ARPIs is when patients first enter advanced PCa. The most cost-effective ARPI at current Canadian prices is abiraterone, mostly due to abiraterone’s lower price level.
Full article
(This article belongs to the Section Health Economics)
►▼
Show Figures

Figure 1

Figure 1
Open AccessArticle
Real-World Treatment Patterns and Outcomes Among Patients with Early Non-Small Cell Lung Cancer
by
Jennifer D. Deem, Zsolt Hepp and Joshua J. Carlson
Curr. Oncol. 2025, 32(4), 239; https://doi.org/10.3390/curroncol32040239 - 19 Apr 2025
Abstract
Worldwide, about two million people are diagnosed with lung cancer each year, 85% of whom have non-small cell lung cancer (NSCLC). Recent progress in treating advanced/metastatic NSCLC with targeted therapies has shifted attention to early NSCLC (Stages I–IIIA) and perioperative (neoadjuvant and adjuvant)
[...] Read more.
Worldwide, about two million people are diagnosed with lung cancer each year, 85% of whom have non-small cell lung cancer (NSCLC). Recent progress in treating advanced/metastatic NSCLC with targeted therapies has shifted attention to early NSCLC (Stages I–IIIA) and perioperative (neoadjuvant and adjuvant) systemic therapies. However, our comprehension of how targeted therapeutics are incorporated into care and their impact on patient outcomes is just starting to unfold. Methods: This retrospective observational study used a US nationwide electronic health record-derived deidentified database spanning January 2019–March 2024 and aimed to describe (1) eNSCLC patient demographic and clinical characteristics, (2) real-world neoadjuvant and adjuvant use, and (3) patient outcomes. Results: The study population included 4841 Stage IB–IIIA NSCLC patients with a mean age of 70.9 ± 8.6 years. The majority (69.9%) received definitive treatment: surgery (n = 2280), definitive radiation (n = 320), or definitive chemoradiation (n = 783), while 30.1% (n = 1458) did not. Many definitive treatment patients received some perioperative systemic therapy (surgery: 52.6%, radiation: 52.2%, chemoradiation: 75.5%). Neoadjuvant use was limited in all groups (surgery: 8.2%, radiation: 6.1%, chemoradiation: 11.6%). Among the 54.6% receiving adjuvant, immune checkpoint inhibitors were the most common choice for definitive radiation (39.1%) and chemoradiation (73.7%) patients, while surgical patients predominantly received platinum-doublet therapy (37.0%). Surgical patient outcomes were similar across all groups, while definitive chemoradiation or radiation patients without systemic therapy had lower survival rates. Conclusions: In this study, we found that although the majority of patients underwent some form of definitive treatment, adjuvant use was limited, and neoadjuvant use was rarely included in care. A crucial initial step in improving patient outcomes is to understand and address the underutilization of neoadjuvant/adjuvant systemic therapy for eNSCLC patients.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures
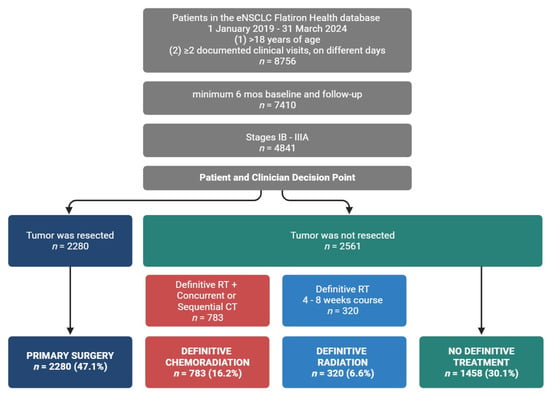
Figure 1
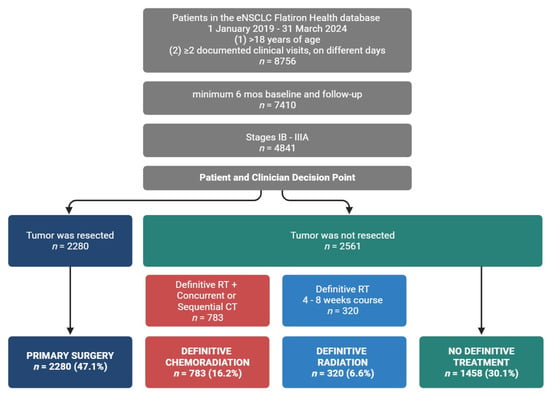
Figure 1
Open AccessReview
Perspectives on Outpatient Delivery of Bispecific T-Cell Engager Therapies for Multiple Myeloma
by
Andrée-Anne Pelland, Mathilde Dumas, Émilie Lemieux-Blanchard, Richard LeBlanc, Julie Côté, Jean-Samuel Boudreault, Dominic Duquette, Rayan Kaedbey, Marc Lalancette, Frédéric Larose, Anna Nikonova, Michel Pavic, April Shamy, Jean Roy, Michael Sebag, Sabrina Trudel and Jean-Sébastien Claveau
Curr. Oncol. 2025, 32(4), 238; https://doi.org/10.3390/curroncol32040238 - 18 Apr 2025
Abstract
In the past few years, a new promising therapy, called bispecific T-cell engager (TCE), has been developed and is now available in many countries for patients with relapsed or refractory multiple myeloma. T-cell engagers are associated with sustained efficacy and progression-free survival benefits
[...] Read more.
In the past few years, a new promising therapy, called bispecific T-cell engager (TCE), has been developed and is now available in many countries for patients with relapsed or refractory multiple myeloma. T-cell engagers are associated with sustained efficacy and progression-free survival benefits in patients with heavily treated myeloma. However, complications such as cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), and infections complicate their administration, particularly in remote centers. This review discusses the key requirements for delivering TCEs therapies, focusing on outpatient delivery. We also outline the primary acute and chronic complications of TCE therapy and their management.
Full article
(This article belongs to the Section Hematology)
►▼
Show Figures
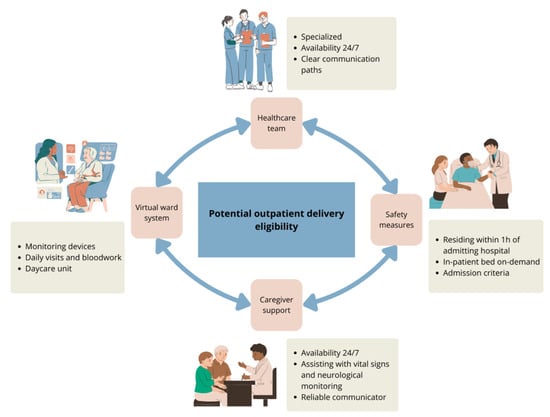
Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Cancers, Cells, JCM, Radiation, Pharmaceutics, Applied Sciences, Nanomaterials, Current Oncology
Innovative Radiation Therapies
Topic Editors: Gérard Baldacchino, Eric Deutsch, Marie Dutreix, Sandrine Lacombe, Erika Porcel, Charlotte Robert, Emmanuelle Bourneuf, João Santos Sousa, Aurélien de la LandeDeadline: 30 April 2025
Topic in
Biomedicines, Current Oncology, Diagnostics, Gastrointestinal Disorders, JCM, Livers, Transplantology
Advances in Gastrointestinal and Liver Disease: From Physiological Mechanisms to Clinical Practice
Topic Editors: Davide Giuseppe Ribaldone, Gian Paolo CavigliaDeadline: 20 June 2025
Topic in
Biomolecules, CIMB, Sci. Pharm., Cancers, Current Oncology, Cells
The Role of Extracellular Vesicles as Modulators of the Tumor Microenvironment
Topic Editors: Nils Ludwig, Miroslaw J SzczepanskiDeadline: 30 June 2025
Topic in
Cancers, Diagnostics, JCM, Current Oncology, Gastrointestinal Disorders, Biomedicines, Therapeutics
Hepatobiliary and Pancreatic Diseases: Novel Strategies of Diagnosis and Treatments
Topic Editors: Alessandro Coppola, Damiano Caputo, Roberta Angelico, Domenech Asbun, Chiara MazzarelliDeadline: 20 August 2025

Conferences
Special Issues
Special Issue in
Current Oncology
Biomarkers and Precision Medicine in Upper Gastrointestinal Malignancies
Guest Editor: Morten LadekarlDeadline: 30 April 2025
Special Issue in
Current Oncology
Cost Effectiveness vs. Affordability in the Age of Targeted Drug Therapies
Guest Editor: Ramy SalehDeadline: 30 April 2025
Special Issue in
Current Oncology
Pediatric Brain Tumors: Advances in Treatment and Patient Outcomes
Guest Editor: Daniele BertinDeadline: 30 April 2025
Special Issue in
Current Oncology
Palliative Care and Supportive Medicine in Cancer
Guest Editor: Daryl BainbridgeDeadline: 30 April 2025
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff










